We Can’t Fight the Next Pandemic with Handouts and Charity to Poor Nations
This op-ed by CMMB president and CEO Mary Beth Powers was originally published in the Miami Herald on December 29th, 2021. Follow Mary Beth on Twitter for more updates and news!
We Can’t Fight the Next Pandemic with Handouts and Charity to Poor Nations
COVID-19 and its never-ending variants have taught us that our global health system is broken.
The charity model to end the pandemic has largely failed. Health inequities between high-income and low-income countries have worsened, and decades of progress in reducing poverty are being reversed. Our global health cooperation system is inadequate and unable to prevent variants from emerging and truly bring the pandemic to an end.
We have to build a more-effective global health infrastructure to ensure we can reduce the impact of COVID-19, and so that we do not make the same mistakes during the next pandemic. We have to develop better supply chains to get medicines and equipment to low-income countries and invest in local manufacturing capability for vaccines and other essential supplies needed. Finally, we have to begin now to train the next generation of skilled healthcare workers.
This isn’t optional. There will be a next pandemic and it may be worse in terms of the case fatality rate of the virus.
COVID-19 is bad, but we caught many breaks. We were fortunate that a tight-knit community of scientists and taxpayer-funded laboratories could develop effective vaccines in record-breaking time. Unlike other viruses, COVID-19 spreads almost exclusively through respiratory droplets. Simple precautions like wearing a mask are effective in preventing viral spread.
“There will be a next pandemic and it may be worse in terms of the case fatality rate of the virus.”
None of those qualities are guaranteed for the next pandemic, which infectious-disease experts say is coming sooner than later.
Defeating COVID-19 and ensuring that the next pandemic does not deal a devastating blow means addressing the gaps found in low-income countries. What does that look like?
It starts with correcting the early failings of the pandemic response. Low-income countries were desperately short of personal protective equipment (PPE) and testing to limit and understand the virus spread. As the southern hemisphere headed into their winter, they lacked not only vaccine doses, but the basics for vaccine distribution, like syringes and adequate refrigeration. These shortages were borne of both weak supply chains and limited supply because of pre-ordering huge volumes of vaccines in high-income countries — some of which went unused and expired.
Public-private partnerships (PPPs) formed by governments, international donors, nonprofits and pharmaceutical companies can help build local capacity to combat COVID-19 and help prepare low-income countries for the next pandemic.
Such PPPs will be a win-win. Low-income countries build local capacity and take ownership over manufacturing, distribution, and supply-chains while pharmaceutical companies gain a foothold and valuable partnerships in new markets.
PPPs have played a key role in tackling previous global health crises, such as HIV/AIDS. The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) utilized PPPs to strengthen logistics and supply chains and HIV lab practices. PEPFAR has played a critical role in prevention of new infections and managing existing infections through effective treatments, saving 20 million lives.
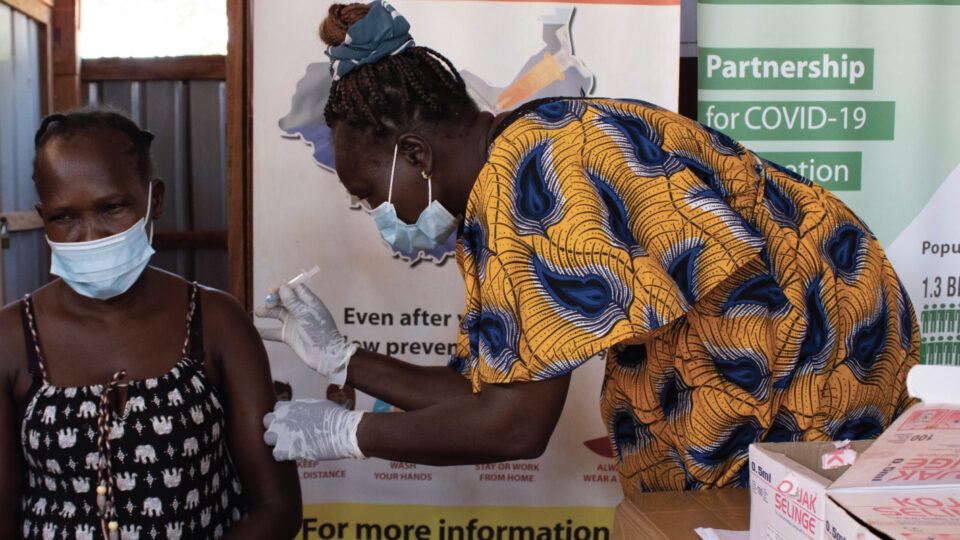
PPPs could form the backbone of developing local vaccine manufacturing and distribution capabilities to get more people vaccinated in low-income countries and save lives. The charity model of high-income countries donating vaccines or funding for vaccines has failed. Just 7.3% of people in low-income countries are fully vaccinated, compared to 56.1% globally. Only 0.8% of all doses delivered have been administered in low-income countries. Africa has the lowest vaccination rate of any continent, with just 11.8% of the population receiving one dose.
As the world faces a global shortage of healthcare workers, there is a desperate need to train and maintain a skilled workforce to fight COVID-19 and any future pandemic. From offering low-interest loans to the cover tuition of aspiring health workers to providing training programs to build local capacity, PPPs can play an integral role in recruiting and training health workers. Low-income countries still lack adequate human resources to administer COVID-19 tests and vaccines. In an emergency, not everyone who administers a test or vaccine needs to be a nurse. People can be quickly trained to provide those crucial services.
PPPs are a better way to mobilize the resources and expertise to distribute some of the building blocks of a global health-security system. Waiting for the handouts or hand-me-downs when it comes to PPE and vaccines is not an effective or equitable way to combat pandemics.
Mary Beth Powers is president and CEO of Catholic Medical Mission Board (CMMB). Follow Mary Beth on Twitter at: twitter.com/MaryBeth_CMMB
